Introduction
- Every year, on December 12, the world observes International Universal Health Coverage (UHC) Day to emphasize the importance of ensuring that all individuals have access to affordable and quality healthcare.
- Rooted in the World Health Organization’s (WHO) 1948 Constitution, UHC highlights health as a fundamental human right and aims for the highest attainable standard of health for everyone.
- Achieving UHC in India, with its diverse population and varying economic backgrounds, presents unique challenges and opportunities.
What is Universal Health Coverage (UHC)?
- The World Health Organization defines Universal Health Coverage (UHC) as “all people having access to the full range of quality health services they need, when and where they need them, without financial hardship.” UHC is underpinned by three essential pillars:
- Access to Health Services: Ensuring that all individuals, regardless of income, can access necessary healthcare services.
- Quality of Services: These services must be effective, safe, and capable of delivering desired health outcomes.
- Financial Risk Protection: No individual should face financial ruin due to healthcare costs.
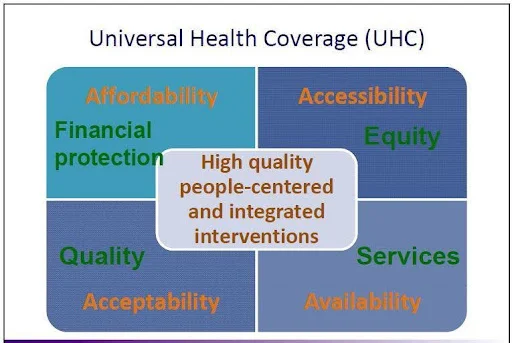
- UHC encompasses the full continuum of essential health services, including health promotion, prevention, treatment, rehabilitation, and palliative care. The aim is to provide inclusive healthcare across all stages of life.
Read also: Impeachment of Judges in India – Process & Provisions | UPSC
Evolution of UHC: A Historical Perspective
- The idea of Universal Health Coverage has evolved over time, influenced by global health movements and significant milestones:
- Alma-Ata Declaration (1978): The World Health Organization’s declaration that “Health for All” should be a global priority.
- Sustainable Development Goals (SDGs) (2015): UHC became a key target in the UN’s 2030 Sustainable Development Agenda under SDG target 3.8. This includes tracking progress through indicators such as essential health service coverage and financial protection.
- Global Action Plan (2019): The first UN High-Level Meeting on UHC led to the adoption of a Global Action Plan, guiding nations to achieve SDG 3.8 and accelerating progress towards UHC.
India’s Commitment to Achieving UHC
- India has committed to achieving UHC through various health policies and programs. The Indian Constitution, through Articles 39(e), 42, and 47, directs the state to improve public health and ensure access to healthcare for all citizens. India has introduced several key initiatives aimed at improving access to healthcare:
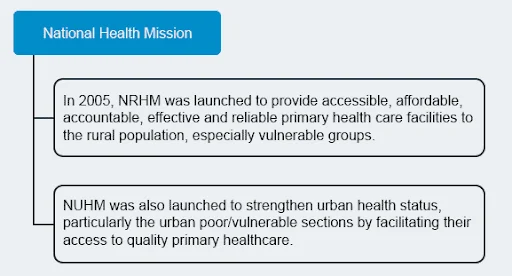
- National Health Mission (NHM): This initiative ensures universal access to affordable and quality healthcare services. As of 2023, over 40 million digital health IDs have been created, paving the way for a more accessible and efficient healthcare system. NHM has two sub-missions:
- National Rural Health Mission (NRHM): Focuses on rural healthcare development.
- National Urban Health Mission (NUHM): Aims to strengthen urban healthcare systems.
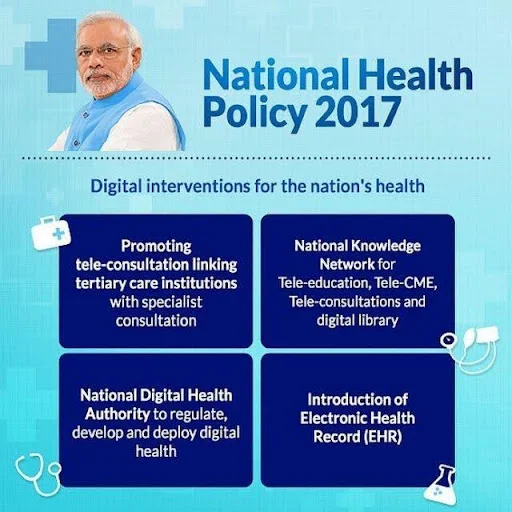
- National Health Policy (NHP) 2017: Aimed at achieving UHC through strengthening primary care, integrating AYUSH (Ayurveda, Yoga, Unani, Siddha, Homeopathy), adopting digital tools, and encouraging public-private partnerships.
- Ayushman Bharat Program: One of India’s flagship health initiatives that seeks to achieve UHC through:
- Health and Wellness Centres (HWCs): Delivering comprehensive primary care services.
- Pradhan Mantri Jan Arogya Yojana (PM-JAY): Providing health insurance coverage of ₹5 lakhs per family annually for secondary and tertiary care.

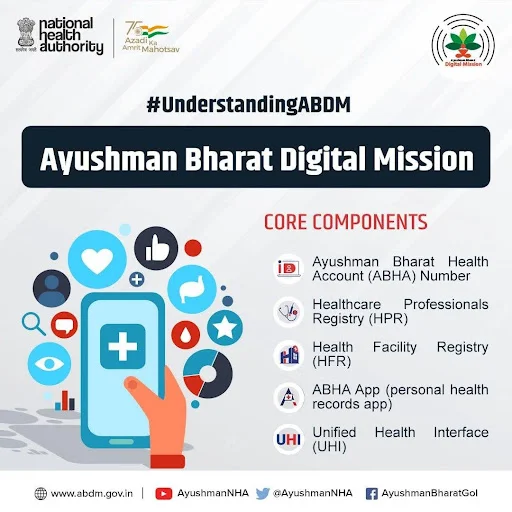
- Ayushman Bharat Digital Mission (ABDM): Enhancing equitable access to healthcare, ABDM promotes digital health technologies such as telemedicine and ensures portability of health services through Ayushman Bharat Health Account (ABHA) numbers.
- Other Key Programs: These include the National Mental Health Programme (NMHP), the National Programme for Health Care of the Elderly, POSHAN 2.0 for improving nutrition, and the Fit India Movement for promoting healthy lifestyles.
India’s Healthcare System: Current State and Key Indicators
- India’s healthcare sector is expansive, though several gaps remain that hinder UHC:
- Market Size and Employment: The healthcare sector is valued at $372 billion (2023) and employs around 7.5 million people. Sub-sectors such as telemedicine and e-health are witnessing rapid growth.
- The telemedicine market in India is expected to grow at a compound annual growth rate (CAGR) of 31.6% between 2020 and 2025. As of 2023, over 8 million virtual consultations are estimated to have been conducted annually in India, showcasing the rapid adoption of digital health solutions.
- Doctor-Population Ratio: India faces a significant shortage of healthcare workers, particularly in rural areas. As per the World Bank, India has just 0.7 nurses per 1,000 people, far below the global average of 2.9 nurses per 1,000 people. With a doctor-to-population ratio of 1:854, India falls short of the WHO-recommended ratio of 1:1000.
- The shortage of healthcare professionals is exacerbated by the uneven distribution, with several states such as Uttar Pradesh and Bihar having fewer healthcare workers per capita than more developed regions like Kerala and Tamil Nadu.
- Medical Tourism: India’s medical tourism sector contributes significantly to the economy, generating $7.69 billion in 2024, with projections to grow to $14.31 billion by 2029. According to the Ministry of Tourism, over 500,000 international patients traveled to India in 2020 alone for medical treatments.
- Health Insurance Penetration: Only 41% of Indian households have health insurance coverage, as per the National Family Health Survey (2019-21).
- Only 16% of rural households in India have health insurance, compared to 61% in urban areas. This leaves a large portion of the population vulnerable to high out-of-pocket expenses for medical treatments, leading to financial distress in many households.
- Healthcare Utilization: Around 48% of Indian households avoid using public healthcare services, primarily due to perceptions of poor quality. According to the NFHS-5, only about 20% of people in rural areas trust government-run healthcare facilities for quality care.
- Non-Communicable Diseases (NCDs) Burden: The burden of non-communicable diseases (NCDs) such as diabetes, hypertension, and cardiovascular diseases is rapidly increasing in India. According to the WHO, NCDs account for nearly 63% of all deaths in India, with lifestyle-related diseases becoming a significant challenge. For example, a study by the Indian Council of Medical Research (ICMR) found that 8.7% of the adult population in India has diabetes, while another 10% are pre-diabetic.
- Mental Health Crisis: Mental health has emerged as a growing concern in India, with the WHO reporting that India has one of the highest rates of mental health disorders globally, particularly among its youth. As of 2021, approximately 14% of India’s population suffers from some form of mental health disorder, including depression and anxiety.
Key Challenges in Achieving UHC in India
- Inadequate Public Health Funding: Despite being the world’s most populous nation, India spends only 1.9% of its GDP on healthcare, well below the WHO’s recommended 3%. This underfunding results in inadequate infrastructure and substandard quality of care.
- For example, India’s healthcare system faces a shortage of hospital beds, with only 0.5 beds per 1,000 people, compared to the WHO’s recommendation of 3 beds per 1,000 people. The lack of funding also contributes to the limited reach of health programs, leaving a vast portion of the population with insufficient healthcare coverage.
- Regional Disparities: Healthcare access remains uneven, with urban areas having superior healthcare facilities compared to rural regions. Despite 65% of the population living in rural areas, 70% of healthcare professionals are located in urban centers.
- For instance, in rural areas, there are fewer than 2 doctors per 10,000 people, while urban areas have over 10 doctors per 10,000 people. This disparity is further compounded by the uneven distribution of healthcare infrastructure, with rural areas often lacking basic medical facilities, leading to delayed access to care, especially in emergencies.
- Weak Primary Healthcare System: Primary healthcare centers (PHCs) are essential for UHC but face challenges such as insufficient funding, poor infrastructure, and limited trust from patients.
- A 2020 report by the National Health Systems Resource Centre revealed that over 50% of PHCs in India lack essential drugs and equipment, and nearly 70% are understaffed.
- Unregulated Private Healthcare Sector: While private healthcare provides a large portion of healthcare services, it is largely unregulated, leading to high treatment costs and unethical practices.
- For example, private hospitals charge up to 10 times more for the same medical procedures compared to public hospitals. A study by the National Institute of Public Finance and Policy (NIPFP) revealed that out-of-pocket expenditures in India account for nearly 60% of healthcare spending, pushing many families into poverty due to high medical costs.
- Focus on Preventive Healthcare: Preventive measures such as immunization and screenings remain underused. According to the National Family Health Survey (NFHS-5, 2021), India’s immunization coverage was only 76.4%, well below the global target of 90%. This means that millions of children are still vulnerable to preventable diseases such as polio, measles, and diphtheria.
- Low Health Awareness: Factors such as low literacy rates and poor awareness about health practices contribute to the underutilization of healthcare services.
- For instance, many women are unaware of the benefits of exclusive breastfeeding, which contributes to malnutrition and stunting in children.
- According to the NFHS-5, only 54.9% of children aged 0-6 months are exclusively breastfed in India.
- This low awareness also extends to other health issues, such as sanitation, hygiene, and the importance of regular health check-ups, leading to poor health outcomes and underutilization of healthcare services.
UPSC Current Affairs: Brahmani River, Standardised Precipitation Index, Bagata Tribe, and More
Way Forward
- Increase Public Healthcare Spending: India needs to allocate 3%-5% of its GDP to healthcare, leveraging public-private-philanthropic partnerships and innovative finance models to boost resources.
- Focus on Preventive Healthcare: Strengthening PHCs and focusing on preventive measures like immunization, screenings, and lifestyle changes can significantly reduce the long-term disease burden and healthcare costs.
- Improve Healthcare Access in Rural Areas: Incentivizing the private sector to invest in healthcare infrastructure in underserved areas, along with tax incentives and rewards for healthcare professionals working in rural regions, can help address regional disparities.
- Expand Health Insurance Coverage: Extending insurance coverage to include outpatient care, diagnostic services for non-communicable diseases (NCDs), and preventive healthcare services will enhance financial protection for citizens.
- Harness Digital Health Solutions: Expanding digital health services like telemedicine and the Ayushman Bharat Digital Mission will increase healthcare access, particularly in remote and underserved areas.
- Integrate Traditional and Modern Healthcare: Combining AYUSH systems with modern healthcare will help relieve pressure on allopathic healthcare providers and provide culturally acceptable care options.
- Regulate the Private Sector: Standardizing healthcare quality reporting across the private sector will improve transparency and reduce exploitation by making healthcare services more accessible and affordable.

