India Fight Against Tuberculosis Introduction
- Every year on March 24, World Tuberculosis (TB) Day is observed to raise awareness about the deadly disease and commemorate the discovery of the Mycobacterium tuberculosis bacterium by Dr. Robert Koch in 1882.
- TB continues to be a significant global health issue, and this day serves as a reminder of the urgent need for collective efforts to combat and eventually eliminate this disease.
- In India, TB remains a major public health challenge. Despite significant progress, the country still carries a large share of the global burden of tuberculosis.
- The “TB Free India Campaign” launched in 2018 aims to eradicate TB by 2025, but to achieve this ambitious goal, India must overcome numerous hurdles. As we observe World TB Day in 2023, it’s crucial to evaluate both the progress made and the obstacles that persist in the battle against tuberculosis.
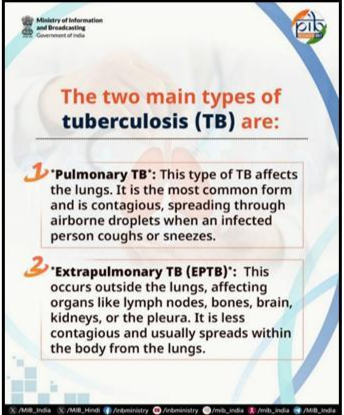
What is Tuberculosis (TB)?
- Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis.
- It primarily affects the lungs but can also damage other parts of the body, including the kidneys, spine, and brain.
- TB is transmitted through the air when an infected person coughs, sneezes, or talks. Left untreated, TB can be fatal, but with proper treatment, it is curable.
- TB remains one of the leading causes of death worldwide, and it is particularly prevalent in low- and middle-income countries like India.
Current Status of Tuberculosis Burden in India
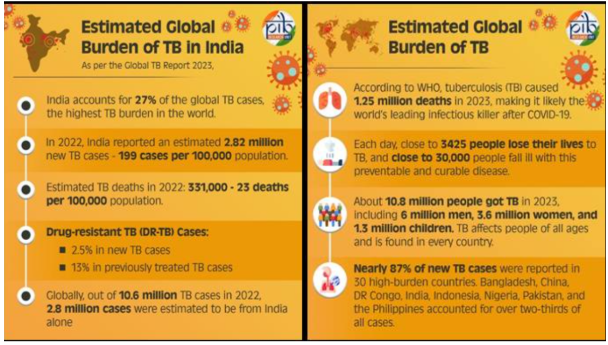
- India continues to bear the highest burden of tuberculosis in the world. Despite improvements in detection and treatment, the numbers are still alarming:
- Record TB Notifications in 2023: India notified 25.5 lakh TB cases in 2023, a significant increase from previous years. Notably, more than 8.4 lakh cases were reported by the private healthcare sector, reflecting greater participation of the private sector in reporting TB cases. This is a 21-fold increase in notifications since 2013, marking a significant step forward in the country’s efforts to combat TB.
- Global TB Burden: According to the WHO Global TB Report 2023, India is home to 27% of the world’s TB cases, with 2.82 million new cases reported in the country. This makes India the epicenter of the global TB epidemic, highlighting the urgent need for continued and enhanced intervention. The WHO report noted that five countries contributed to 56 percent of the worldwide TB cases—India (26 percent), Indonesia (10 percent), China (6.8 percent), the Philippines (6.8 percent), and Pakistan (6.3 percent).
Why is Eliminating Tuberculosis Crucial for India?
- Improved Public Health: TB remains one of the leading causes of illness and death in India. This has a direct impact on the health of the nation, and eradicating TB would reduce these preventable deaths significantly. India’s National TB Prevalence Survey 2019-2020 found that the national TB prevalence rate is 2.1 million cases, and without further intervention, this number could continue to rise. Eradicating TB would vastly improve public health by reducing mortality rates and preventing new infections.
- Economic Consequences: TB poses a significant economic burden on India, impacting individuals and the national economy.
- A study published in the Lancet Global Health Journal (2019) revealed that the economic cost of TB in India is approximately $23.8 billion annually, which is about 1.1% of India’s GDP. The study found that the disease leads to loss of income, reduced productivity, and increased healthcare costs, especially among economically disadvantaged groups. By eliminating TB, India can save these costs and prevent further economic loss, resulting in an overall improvement in economic health.
-
-
- The World Bank also estimates that TB-related illness and death could cause up to $16 billion in lost productivity annually in India. Reducing TB cases will allow individuals to remain productive members of the workforce, thereby contributing to the country’s economic growth.
-
- Poverty Reduction: TB disproportionately affects people living in poverty. The Indian Council of Medical Research (ICMR) has highlighted that TB is more common in overcrowded living conditions, and among those who lack access to quality healthcare and suffer from malnutrition.
- The Lancet Infectious Diseases Journal (2021) shows that TB is both a cause and a consequence of poverty, where people living in poverty are more likely to contract the disease, and those who fall ill are pushed further into economic hardship due to the high cost of treatment.
-
-
- The TB Free India Campaign (launched in 2018) has made significant strides in improving the accessibility and affordability of TB treatment, especially in poor communities. This can help address the health disparities that exacerbate poverty in affected populations.
-
- Global Health Contribution: TB is a global health challenge, and India’s success in eliminating TB would have a significant impact on global efforts to eradicate the disease.
- A study by the Global Fund (2020) showed that India’s efforts toward TB eradication directly contribute to the global target of reducing TB incidence by 90% by 2035.
- Since India accounts for a substantial percentage of global TB cases, eliminating the disease within the country would significantly reduce the global TB burden and set an example for other nations to follow.
- Achievement of Sustainable Development Goals (SDGs): The elimination of TB is a key target under the United Nations’ Sustainable Development Goals (SDGs), particularly SDG Goal 3, which aims to ensure healthy lives and promote well-being for all.
- According to the WHO Global TB Report 2021, India has committed to ending the TB epidemic by 2025, in line with the global TB elimination target under SDG 3.3.
-
-
- The Indian government’s TB Free India Campaign, which aims to eradicate TB by 2025, aligns with SDG targets and contributes directly to improving health and reducing inequalities in India. Achieving TB elimination would not only benefit India but also set a precedent for other countries to follow, especially those with a high burden of TB.
-
- Social Justice: TB disproportionately affects marginalized and vulnerable populations, including low-income groups, women, children, and those with limited access to healthcare.
- Studies by the UNDP have shown that TB patients from marginalized groups are more likely to face discrimination and social exclusion, which further deepens their health and socio-economic challenges.
-
- TB Free India Campaign has made significant progress in addressing the social determinants of TB, such as poor living conditions and lack of awareness. By focusing on vulnerable populations and ensuring they have access to healthcare, India is moving towards a more equitable society.
What are the Challenges in Eliminating Tuberculosis in India?
- High Burden of TB Cases: India carries the largest burden of TB in the world, accounting for 28% of the total TB cases globally, according to the Global TB Report 2022.
- In 2021, India reported 25.9 lakh TB cases, a figure that underscores the enormity of the epidemic. This sheer volume of cases makes it difficult to identify and treat all patients in a timely manner.
- With such a high number of cases, India struggles to ensure early detection, proper treatment, and complete adherence to treatment regimens.
-
-
- A report from the Indian Council of Medical Research (ICMR) estimates that nearly 50% of TB cases go undiagnosed in India. Many cases, particularly in rural areas, remain undetected due to poor surveillance, leading to untreated TB spreading further within communities.
- Drug-Resistant TB: India faces a high burden of drug-resistant TB (DR-TB), which is far more difficult and expensive to treat than regular TB. India also has the highest number of multi-drug-resistant TB (MDR-TB) cases worldwide.
-
- In 2020, the WHO Global TB Report noted that India had around 1.2 lakh cases of drug-resistant TB. These cases arise due to the misuse of antibiotics, poor adherence to treatment regimens, and incomplete treatment courses, leading to the development of resistant strains.
-
-
- The National Institute for Research in Tuberculosis (NIRT) reports that in India, multidrug-resistant TB (MDR-TB) accounts for about 2% of all new cases and 15% of previously treated cases. The treatment for drug-resistant TB can last up to 2 years, is more costly, and has higher rates of treatment failure compared to regular TB, posing a serious challenge to eradication efforts.
-
- Limited Access to Healthcare: Many individuals, especially those in rural areas, face significant barriers to accessing quality healthcare. Long travel distances to reach healthcare centers, high treatment costs, and limited availability of healthcare workers in remote regions result in delayed diagnosis and treatment, exacerbating the spread of TB. This is particularly true for those in tribal and remote rural populations.
-
-
- According to the World Health Organization’s (WHO) report on TB in India, more than 70% of the TB burden is concentrated in rural areas where access to healthcare facilities is inadequate. For instance, rural Maharashtra faces challenges in treating TB patients due to a lack of diagnostic facilities, and patients often delay seeking care due to financial constraints.
-
- Stigma and Discrimination: The social stigma surrounding TB continues to be a major hurdle in controlling its spread. Many people with TB are reluctant to seek treatment due to the fear of discrimination, social isolation, and loss of employment. This stigma can prevent individuals from disclosing their condition and seeking medical help, thus increasing the spread of TB within communities.
-
-
- The TB Stigma Survey conducted by The Union and partners revealed that more than 50% of TB patients reported facing discrimination due to their condition, especially in urban slums. Patients are often afraid of being ostracized by family members, neighbors, and even healthcare providers, which results in delays in seeking treatment and incomplete treatment courses.
-
- Poor Living Conditions: Overcrowded housing, poor sanitation, and lack of clean water are significant factors contributing to the transmission of TB. These conditions are especially prevalent in urban slums and rural areas, where large populations live in close proximity, increasing the risk of airborne diseases like TB.
-
-
- Dharavi, one of Mumbai’s largest slums, has been identified as a major hotspot for TB transmission due to its high population density, poor sanitation, and inadequate healthcare access.
- In 2020, a study by the BMC Public Health found that over 60% of residents in Dharavi were unaware of the risks of TB, and the overcrowded conditions made it a perfect environment for the disease to spread.
-
- Limited Awareness: Many people in India still lack awareness about the signs and symptoms of TB, the importance of completing the full course of treatment, and the availability of free treatment options through government programs. Delayed diagnosis and treatment discontinuation are common problems, which not only hinder the control of TB but also increase the risk of drug-resistant TB strains developing.
-
-
- According to the National TB Elimination Program (NTEP) data, around 50% of TB patients in rural areas are unaware of the free treatment options available through government-run TB programs. This lack of awareness leads to delayed healthcare seeking and contributes to a higher transmission rate in the community.
-
- Insufficient Funding and Resources: Despite TB being a major health problem in India, it has historically received insufficient funding. While the government has increased allocations to TB control programs, the financial and logistical resources dedicated to tackling the disease remain inadequate. Limited infrastructure, shortage of healthcare professionals, and ineffective policy execution further hinder the country’s progress in TB elimination.
-
- The Global Fund estimates that India needs $2.6 billion in funding annually to combat TB effectively. However, funding from both government and private sectors is still far from sufficient. For example, in 2019, India allocated only $182 million for TB programs, falling short of the required investment to control the epidemic effectively.
Government’s Key Initiatives for TB Elimination in India
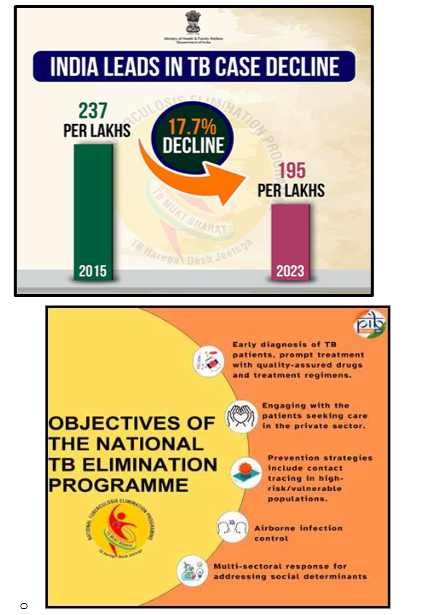
- National TB Elimination Programme (NTEP): The National TB Elimination Programme (NTEP) is the cornerstone of India’s strategy to make the country TB-free by 2025, ahead of the global 2030 target.
-
- One of its key achievements has been reducing the number of missing TB cases from 15 lakh in 2015 to just 2.5 lakh in 2023 with a decrease of 83%.
- Under NTEP, India has rolled out improved drug-resistant TB treatments, including a safer, shorter all-oral Bedaquiline regimen, boosting success rates from 68% (2020) to 75% (2022).
- Under the NTEP, the incidence rate of TB cases have dropped by nearly 17.7%, from 237 cases per 1 lakh people in 2015 to 195 in 2023.
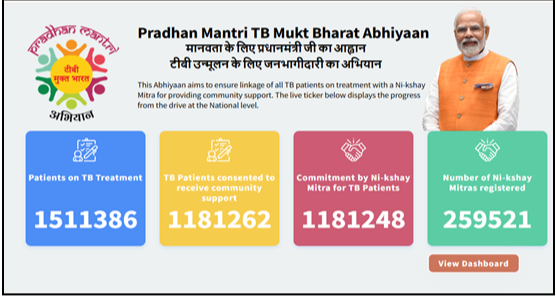
- PM TB Mukt Bharat Abhiyaan (2022): Launched in 2022, the PM TB Mukt Bharat Abhiyaan aims to accelerate TB elimination by promoting community participation, introducing advanced diagnostics, improving treatment protocols, and fostering innovative solutions.
- This program focuses on mobilizing CSR contributions from businesses and institutions.
- The PM TB Mukt Bharat Abhiyaan encourages local community leaders and healthcare workers to take active roles in encouraging people to get screened for TB, especially in high-burden districts, such as Madhya Pradesh and Uttar Pradesh.
- PMTBMBA is also recognized as the world’s largest crowd-sourcing initiative for nutritional support to TB patients.
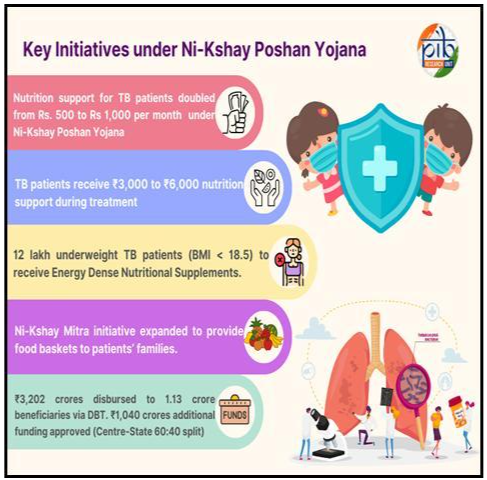
- Ni-Kshay Mitra Initiative : Under the Pradhan Mantri TB Mukt Bharat Abhiyaan (PMTBMBA), the Ni-Kshay Mitra initiative encourages individuals, NGOs, corporates, faith-based organizations, and others to adopt TB patients for at least six months, offering them nutritional, social, or economic support. Over 1.51 crore TB patients are receiving treatment, with approximately 1.18 crore consenting to receive support. Around 1.18 crore commitments have been made by Ni-kshay Mitras, and over 2.59 lakh Mitras are registered.
- Ni-kshay Portal: Ni-kshay Portal is a web-based system under NTEP for TB patient management and surveillance. Developed by the Central TB Division, MoHFW, with NIC and WHO India, it enables health workers to register cases, order tests, track treatment, and monitor adherence. It also functions as India’s National TB Surveillance System, ensuring real-time data reporting.
- Introduction of CB-NAAT and TrueNat for TB Detection: The government has increased access to advanced molecular diagnostic tests such as CB-NAAT (Cartridge-Based Nucleic Acid Amplification Test) and TrueNat to improve TB detection, especially in rural areas. These rapid diagnostic tests help in detecting TB and drug resistance more quickly, allowing for earlier treatment and preventing the spread of the disease.
-
-
- In 2020, the government expanded the use of TrueNat machines in rural districts, increasing the detection rate by 30% compared to traditional methods. These machines are portable, allowing for diagnostic testing in remote villages.
- Ni-Kshay Poshan Yojana (NPY): Provides financial support for TB patients’, nutrition has been increased from ₹500 to ₹1,000 per month, providing ₹3,000 to ₹6,000 per patient throughout treatment.
-
- Improvements in Treatment Protocols: India has made significant strides in improving its TB treatment protocols. Injectable kanamycin, which caused severe side effects like kidney failure and deafness, has been replaced with Bedaquiline and Delamanid for drug-resistant TB (DR-TB) patients. These newer medications have fewer side effects and are also included in the National List of Essential Medicines, allowing the government to regulate their pricing for better access.
-
- A study by the Indian Council of Medical Research (ICMR) found that patients treated with Bedaquiline experienced higher success rates and fewer complications compared to those who used kanamycin-based regimens.
Private Sector Involvement in TB Treatment
- Public Private Interface Agency (PPIA): The Public Private Interface Agency (PPIA) acts as an intermediary between the national TB program and private healthcare providers. It helps ensure that private practitioners adhere to the Standards of TB Care in India, improving the quality of TB care across the country.
- Engaging with Private Healthcare Providers: To ensure high-quality care for TB patients, the Indian government has partnered with private healthcare providers. These partnerships ensure that private doctors and clinics adhere to the national TB care guidelines and standards for diagnosis and treatment, leading to better care and outcomes.
-
-
- In Delhi, private clinics are now required to report TB cases to the National TB Program, helping bridge the gap between the private and public sectors in delivering comprehensive care.
-
- Patient Provider Support Agency (PPSA): The Patient Provider Support Agency (PPSA) connects private healthcare providers, such as medical practitioners, chemists, laboratories, and corporate hospitals, with the National TB Elimination Program. This network ensures that all healthcare professionals in the private sector comply with national treatment protocols and contribute to reducing TB transmission.
- Example: In Chennai, the PPSA has improved diagnostic practices in private clinics, ensuring early detection of TB and proper treatment.
What Should Be the Way Forward?
- Engaging Better with Private Chemists: Retail chemists are often the first point of contact for patients, particularly in rural areas. Training chemists to monitor the H1 schedule and restricting over-the-counter sales of antibiotics will help reduce the misuse of antibiotics and curb the development of drug-resistant TB.
- Leveraging the Network of Rural Medical Practitioners: Rural medical practitioners and village doctors have a high degree of trust within their communities. The government should leverage this network to improve TB detection and early diagnosis, especially in underserved areas where access to formal healthcare is limited.
- Implementation of a Comprehensive TB Control Program: India should develop and implement a comprehensive TB control program that addresses all aspects of the TB lifecycle — from early diagnosis and treatment to follow-up care and prevention. This approach should include collaborations between public health authorities, private healthcare providers, and community organizations to create a holistic TB care model.
- Investment in Research and Development: Increasing investment in research and development (R&D) is essential for identifying new diagnostic tools and effective treatments. Recent developments like the AI-powered software for digital chest X-rays show promise in identifying TB hotspots in the lungs, providing a cost-effective and efficient method for active TB case finding. AI-based software, such as the one developed by IIT Delhi and AIIMS, is being used to detect TB lesions in digital X-rays. This could revolutionize mass screening efforts and speed up TB diagnosis.
- Increased Government Funding: TB prevention and treatment should be prioritized in terms of funding. The government must increase financial allocations to TB research, public awareness programs, TB treatment initiatives, and national TB elimination efforts. A report by the Global Fund has urged India to increase its TB funding to ensure that the elimination goal by 2025 is met. This funding should be targeted toward innovative treatments, scalable diagnostics, and community outreach programs.